Epidemiology:
- Relatively uncommon with proper aseptic technique;
- higher risk in immunocompromised patients, smokers, or those with poor oral hygiene.
Expected Prognosis:
- Generally good with prompt diagnosis and treatment;
- delayed care may prolong healing and cause complications.
Natural Progression:
- Begins with localized redness, swelling, pain; may progress to pus discharge,
- systemic symptoms (fever), and spread to adjacent tissues.
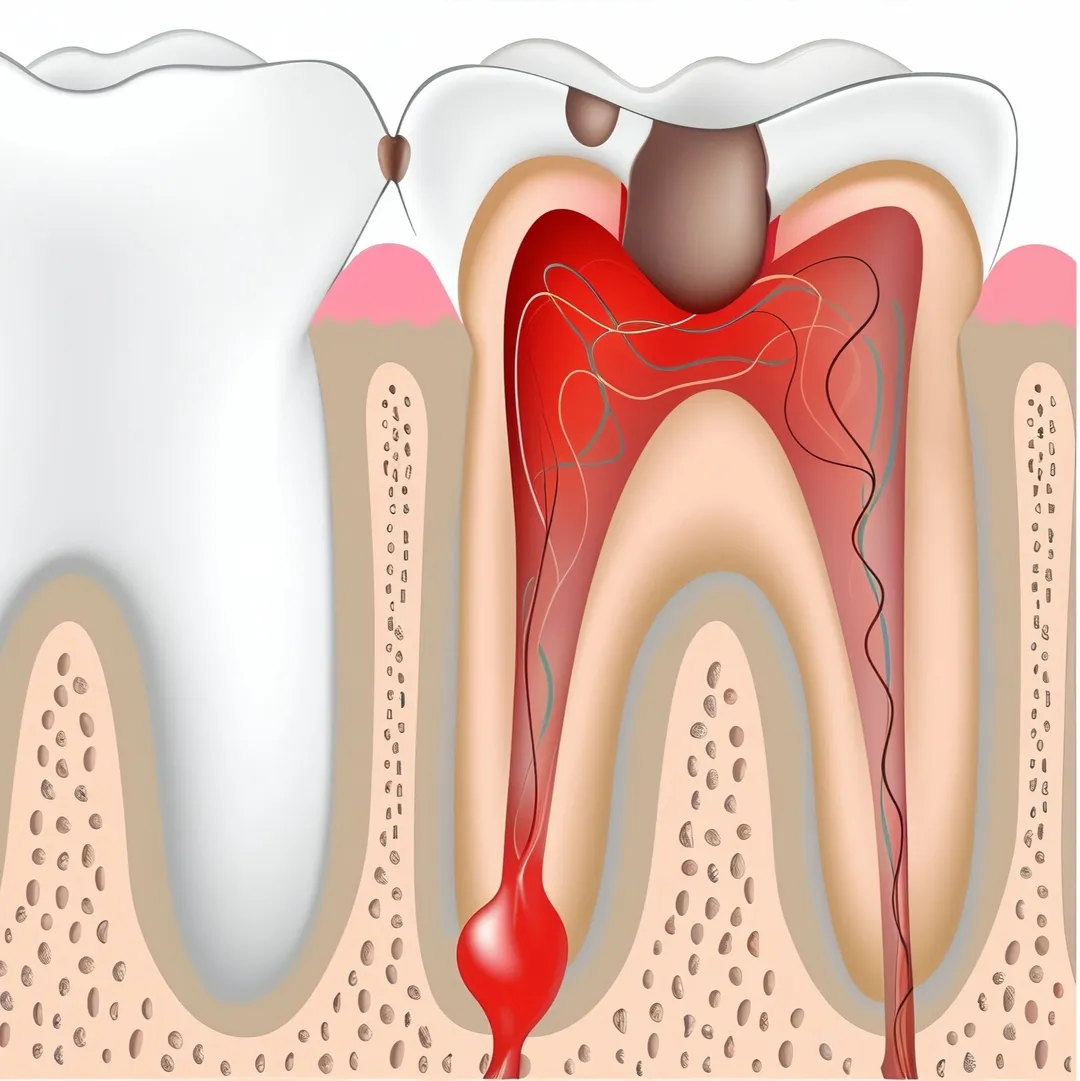
Pathophysiology:
- Bacterial invasion of surgical/debrided site due to tissue trauma, reduced immune defense,
- or residual plaque/biofilm; triggers inflammatory response and pus formation.
Possible Complications:
- Cellulitis, abscess, osteomyelitis, delayed wound healing, systemic spread (sepsis),
- or recurrence of periodontal disease.
Frequently Asked Questions
What causes infections after dental procedures?
Infections can occur if bacteria enter the surgical site, especially after extractions, implants, or root canals. Poor oral hygiene and weakened immunity also increase the risk.
What are the symptoms of a dental infection?
Symptoms include swelling, pain, pus formation, bad breath, fever, and difficulty opening the mouth.
How are dental infections treated?
Treatment may involve antibiotics, draining the infection, or further dental procedures like root canals or extractions.
Can the infection spread to other parts of the body if leaft untreated?
Yes, if left untreated, the infection can spread to the jaw, sinuses, and even vital organs, leading to serious complications.
How can I prevent dental infections?
Maintain good oral hygiene, follow post-treatment care instructions, and visit your dentist regularly for check-ups.
Infection can be an adverse outcome of

Root Canal Treatment
Root canal is a treatment to repair and save a badly damaged or infected tooth instead of removing it. The term "root canal" comes from cleaning of the canals inside a tooth's root.

Inlays and Onlays
Inlays and onlays are conservative, custom-made restorations designed to repair moderately damaged teeth while preserving their natural structure.

Dental Fillings
Dental fillings, whether made of composite resin or glass ionomer cement (GIC), are effective solutions for restoring teeth affected by decay, fractures, or wear.

Dental Implants
Dental implants are a gold standard for tooth replacement, offering a durable, natural-looking and functional solution.

Dental Implant Fixing
Dental implant fixing is a highly durable and effective solution for replacing missing teeth.

Surgical Extraction
Surgical extraction is a necessary procedure for removing teeth that are impacted, decayed, or damaged beyond repair.

Wisdom Tooth Extraction
Wisdom tooth extraction is a common surgical procedure to remove problematic or impacted third molars.

Oral Cancer Screening
Oral cancer screening is a vital tool for early detection of precancerous or cancerous conditions in the oral cavity.